Continuous Quality Improvement
Continuous Quality Improvement (CQI) refers to the structured processes used within the pharmacy, which allows for continual review and improvement of all aspects of the medication dispensing process, to improve patient safety. It is about change and increasing the chances that the changes made in pharmacy result in improved patient safety. To achieve safer care for patients, CQI must focus on both system improvements as well as the tasks performed within each pharmacy.
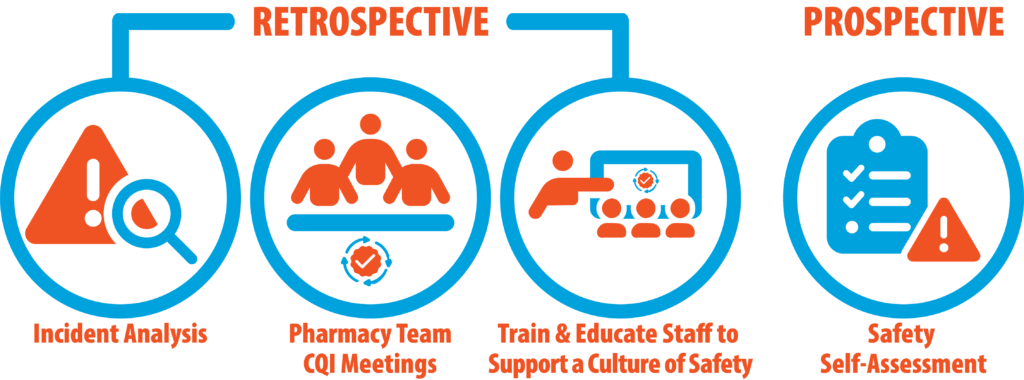
CQI is an ongoing, collaborative, and iterative process and may be retrospective or prospective.
Continuous Quality Improvement Coordinator
Although it remains the pharmacist-in-charge's (PIC) responsibility to ensure the pharmacy complies with the MedSTEP NL program requirements, a PIC may appoint a member of the pharmacy team as the Continuous Quality Improvement (CQI) Coordinator. The CQI Coordinator's responsibilities may include:
- assisting with the development and updating of the pharmacy's policy and procedure manual for CQI and Medication Incident Reporting (MIR);
- ensuring staff are trained on the use of the pharmacy's chosen medication incident reporting platform;
- ensuring incidents and near-misses are consistently reported and discussed;
- promoting a culture of safety and fostering open communication about incidents and safety concerns;
- leading CQI meetings or informal huddles;
- conducting the Safety Self-Assessment (SSA) with other pharmacy staff; and/or
- educating staff about safe medication practices and other safety issues.
Continuous Quality Improvement Meetings
Continuous Quality Improvement (CQI) meetings are an opportunity to educate on medication safety and encourage open dialogue with all pharmacy team members to foster a culture of safety and a team-based approach to CQI and medication incident reporting (MIR). Open communication and discussion with the pharmacy team drive change that improves patient safety.
CQI meetings are a mandatory requirement of MedSTEP NL. NLPB's Standards of Practice for Continuous Quality Improvement and Medication Incident Reporting require formal documented CQI meetings at least every 6 months with informal huddles occurring as medication incidents or near-miss events occur. These meetings should include:
- Review the pharmacy's safety self-assessment.
- Review the pharmacy's incident data summary for trends and discussion of potential issues.
- Discuss summary reports and analyses of pharmacy-specific data, and shared learning from the National Incident Data Repository, ISMP Canada, and NLPB.
- Discuss medication incidents and near-miss events.
- Discuss the progress of existing improvement plans and create improvement plans based on medication incidents and near-miss events.
- Share learning and staff education on medication safety.
The pharmacist-in-charge is responsible for ensuring that a documentation process for formal CQI meetings with pharmacy staff, including meeting dates, staff members present, topics of discussion, and shared learning, is in place.
Culture of Patient Safety
A culture of patient safety is a component of organizational culture, which includes the shared beliefs, attitudes, values, norms, and behavioural characteristics of employees, and influences staff member attitudes and behaviours in relation to their organization's ongoing patient safety performance. An enabling patient safety culture is characterized by leadership that leads by example, transparent communications, psychological safety, facilitating reporting errors, patient and family engagement, and a commitment to ongoing improvement.
Safety Self-Assessment
A safety self-assessment (SSA) is a process used by pharmacy professionals to proactively identify potential safety concerns. Regular use of this process may help decrease the number of medication incidents and near misses and identify opportunities for improvement at a pharmacy to mitigate risks to patients.
A pharmacy-specific SSA is a requirement for pharmacies under the Standards of Practice for Continuous Quality Improvement and Medication Incident Reporting. A pharmacist-in-charge (PIC) must ensure that a pharmacy-specific SSA is completed:
- for an existing pharmacy - during the first year of the MedSTEP NL program, and at least every two years thereafter;
- for a new pharmacy - within the first year of operation, and at least every two years thereafter; and
- within six months following a change in the pharmacy's PIC. In these cases, the outgoing PIC should share the most recent SSA with the new PIC.
An SSA is a tool specifically for pharmacy staff to systematically reflect on the many steps of medication use processes and set measurable goals for quality improvement and should be completed with the involvement of a variety of pharmacy team members. A pharmacy review by corporate or regional staff does not satisfy the SSA requirement for MedSTEP NL.
The PIC is responsible for ensuring an SSA is sourced and completed. Your chosen medication incident reporting (MIR) platform may or may not offer an SSA as part of its service. Two examples of MIR platform providers that offer an SSA as a stand-alone product are:
- ISMP Canada's Medication Safety Self-Assessment for Community/Ambulatory Pharmacy;
- Pharmapod's Pharmacy Safety Self-Assessment;
If your reporting platform does not offer an SSA, please refer to the products listed above to subscribe to a stand-alone product that meets your needs.