Medication Incident Reporting
A medication incident is any preventable event that may cause or lead to inappropriate medication use or patient harm that has reached the patient. Medication incidents may be related to professional practice, drug products, procedures, and systems, and include prescribing, order communications, product labelling/packaging/nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and use. *
All medication incidents that reach a patient need to be reported anonymously to the National Incident Data Repository and should be documented fully in pharmacy records.
Appendix B of NAPRA Model Standards of Practice for Continuous Quality Improvement and Medication Incident Reporting provides a list of levels of harm.
Near-miss
A near miss is an event that could have resulted in unwanted consequences but did not reach the patient either by chance or through timely intervention. *
Near misses create opportunities to analyze medication system processes, enabling a better understanding of potential gaps in existing systems which can then be addressed before an actual medication incident occurs.
The pharmacist-in-charge is responsible for establishing policies and procedures related to the documentation and reporting of near-miss events including:
- documenting the near miss using the pharmacy’s reporting platform;
- determining if the near miss must be reported to the national database according to the pharmacy’s policies and procedures; and
- when required, submitting a report of the near miss to the national database using the pharmacy’s reporting platform.
Appendix A of the NAPRA Model Standards of Practice for Continuous Quality Improvement and Medication Incident Reporting provides a list of sample criteria that may be used to determine whether a near miss should be reported to a national/provincial database and includes
- Were it to reach the patient, the near miss may cause harm.
- The near miss has been a recurrent issue in the pharmacy.
- The near miss provides a learning opportunity for the pharmacy or for pharmacy practice in general.
*Definitions provided by: https://ismpcanada.ca/resource/definitions-of-terms
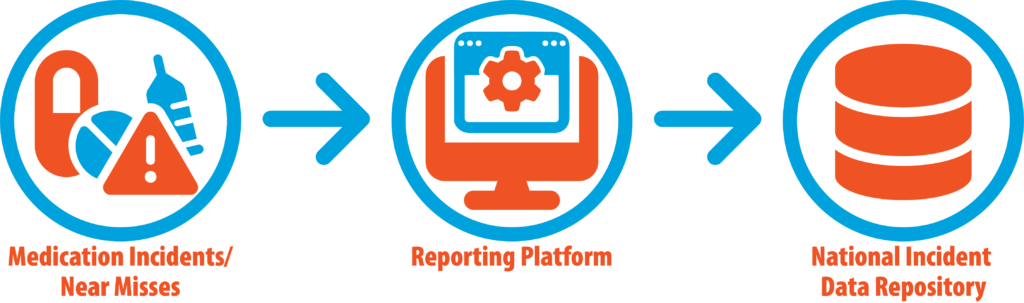
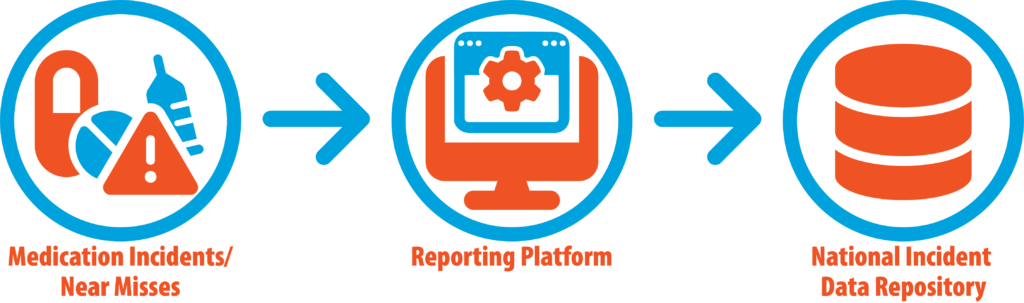
Reporting Process
As per the Standards of Practice for Continuous Quality Improvement and Medication Incident Reporting in Community Pharmacies (Standards of Practice for CQI and MIR), pharmacy professionals are required to document medication incidents and specific near-miss events in the pharmacy and submit a report to the National Incident Data Repository (NIDR) using the pharmacy’s reporting platform.
NATIONAL INCIDENT DATA REPOSITORY (NIDR)
The NIDR for Community Pharmacies, which is a component of the Canadian Medication Incident Reporting and Prevention System (CMIRPS) has been designated by NLPB as the national database for the mandatory reporting of medication incidents and near misses. The CMIRPS’ NIDR is a repository of medication and near-miss reporting data submitted across Canada. The data contained in the national database is de-identified (anonymous) of both patient and healthcare provider professionals’ personal information.
Submission of incident and near-miss information to the NIDR helps to create a national information-sharing system that facilitates the understanding of medication incidents and near-misses across the profession and supports the development of strategies and recommendations to prevent patient harm.
For more information, please refer to the ISMP CANADA NIDR FAQ.
MEDICATION INCIDENT REPORTING (MIR) PLATFORM
A Medication Incident Reporting (MIR) platform is a software program used by pharmacy professionals for recording medication incidents and near misses at the pharmacy level and submitting them to the NIDR. All community pharmacies are required to implement a MIR Platform that meets the requirements outlined in the Standards of Practice for CQI and MIR and fulfills the MedSTEP NL MIR platform criteria.
For a Medication Incident Reporting (MIR) platform to meet the criteria of the MedSTEP NL program it must:
- Submit all reported medication incidents/near-misses into the National Incident Data Repository (NIDR).
- Allow more than one user to add details pertaining to the same incident/near-miss.
- De-identify and anonymize all data submitted to the NIDR (no patient identifiers nor identifiers of pharmacy staff reporting or involved in the incident).
- Produce online and real-time summary reports for the pharmacist-in-charge.
- Provide online tools for documenting improvement plans.
- Include an online module accessible to all pharmacy staff on how to use the platform for shared contributions when reporting.
- Provide MIR training resources and tools as well as ongoing support and communication to pharmacies.
- Provide responsive technical support services that pharmacy staff can readily access.
The following Medication Incident Reporting (MIR) platforms are currently reporting in the National Incident Data Repository (NIDR):
If you wish to use an alternative reporting platform (e.g., developed in-house or corporate), please ensure it meets the requirements outlined in the Standards of Practice for Continuous Quality Improvement and Medication Incident Reporting and fulfills the MedSTEP NL MIR platform criteria.
The following fields are mandatory for submission to the National Incident Data Repository (NIDR):
- Date incident/near-miss occurred
- Type of incident
- Incident discovered by (anonymous, i.e. pharmacist, registered pharmacy technician, patient, other)
- Medication system stages involved in this incident
- Medication (s) involved
- Degree of harm to patient associated with incident
- Incident description/how the incident was discovered
The following fields are optional for submission to the NIDR:
- Time incident occurred
- Patient's gender
- Patient's age
- Other incident information
- Contributing factors to this incident
- Actions at the pharmacy level (including the action plan, the person in charge, and the target date for completion)
- Shared learning for ISMP Canada to disseminate (What has been done to prevent a similar occurrence in the future)
- Review:
- Choose a Medication Incident Reporting (MIR) Platform.
Choose a platform provider that meets the requirements outlined in the NLPB's Standards of Practice for CQI and MIR and fulfills the MedSTEP NL MIR platform criteria. There are several MIR platforms currently reporting to the National Incident Data Repository (NIDR).
- If your pharmacy is part of a corporation that already subscribes to a reporting platform, make sure the platform meets the requirements outlined in NLPB's Standards of Practice for CQI and MIR and fulfills the MedSTEP NL MIR platform criteria. Once confirmed, proceed to Step 3.
- Otherwise, you may choose any reporting platform that meets the MedSTEP NL requirements.
Platform providers will work with ISMP Canada to work on data submission and mapping technology to allow for the export of incident/near-miss data in an acceptable format to the NIDR.
- Sign a data sharing agreement with ISMP Canada between the data owner (pharmacist-in-charge) and the NIDR (housed by ISMP Canada).
- The data-sharing agreement will name your selected reporting platform.
- Contact the NIDR team at NIDR@ismpcanada.ca to start the process
Please note that NLPB will not be approving reporting platform providers. It is the responsibility of the pharmacist-in-charge as the pharmacy license holder to ensure that the chosen platform meets the MedSTEP MIR platform criteria.
ISMP Canada has a Privacy Policy. In accordance with the policy, the data submitted to the National Incident Data Repository (NIDR) is used by ISMP Canada only for the purposes of analysis, recommended actions to improve medication safety, and shared learning.
Pharmacists-in-charge (PICs) and applicable Medication Incident Reporting (MIR) Platform providers submitting incident data are responsible for ensuring that all identifying information is removed before submission to the NIDR.
NLPB will not have access to individual incident submissions from the MIR to the NIDR. NLPB will receive de-identified aggregate data summaries from the NIDR to review provincial medication incident trends.
To evaluate the engagement of pharmacies in the roll-out of the MedSTEP NL program and beyond, NLPB may ask platform providers to provide de-identified data on the number of pharmacies that have reported an incident or near-miss event and the date of the last report for each de-identified pharmacy.
In addition, to evaluate pharmacy compliance with MedSTEP NL implementation, ISMP Canada may share with NLPB which pharmacies have signed a data-sharing agreement. The NLPB will assess how pharmacies utilize and engage with MedSTEP NL during routine practice site inspections.